World Mosquito Day

On August 20, 1897, British doctor Sir Ronald Ross discovered that the female Anopheles mosquito transmits the malaria parasite between humans. Today we commemorate the groundbreaking discovery as World Mosquito Day.

Nearly half of the world’s population is at risk of contracting malaria (World Health Organization, 2016).
Mosquitoes are often attributed as being the world’s deadliest creatures, as they are one of nature’s most notorious vectors for human and zoonotic diseases. Almost 700 million people contract a mosquito-borne illness annually, resulting in over one million deaths. Prominent pathogens include yellow fever, dengue, chikungunya, and malaria. Malaria in particular is the focus of much international concern because it alone causes 216 million cases across 91 countries—and a resounding 445,000 deaths as of 2016 (World Malaria Report, 2017)!
There has been significant progress in malaria control and elimination in the last 121 years since Sir Ronald Ross’ discovery: the creation of Chloraquin in 1934, the testing of the insecticide DDT in 1939, the prophylaxis medication Mefloquine in 1989, and a vaccine in 1992. However, through long lasting insecticide treated net (LLIN) distributions, indoor residual spraying (IRS) campaigns, and a vaccine roll-out, there has been an increase in drug resistant malaria in Southeast Asia.

Cambodia is the epicenter of drug-resistant malaria. This parasite is resistant to artemisinin, the most common antimalarial medication.
PfD has been taking an active role in the fight to contain drug-resistant malaria in Cambodia since 2004. Through the Regional Artemisinin Initiative (RAI) and collaboration with the University Research Company on the Malaria Control in Cambodia (MCC) project, PfD spreads knowledge and resources to rural communities in 11 provinces. This is absolutely critical, as roughly 44% of the country’s population resides in high malaria transmission risk zones.
With the goal of combating the spread of drug-resistant malaria, PfD has placed an emphasis on institutional capacity building, disseminating malaria knowledge, and increasing access to malaria diagnosis and treatment services. While these activities from PfD have decreased malaria incidence, the fight is far from over.
You can help out by sharing this blog post on social media! Or, why not call your congressman or woman to support the Global Fund to Fight AIDS, Tuberculosis, and Malaria? We hope you join us to stamp out malaria!


In Cambodia, there have been great gains in reducing the morbidity and fatality of malaria. In 2015 there were only 10 reported deaths from malaria. Over 80% of cases occurred amongst people age 15-49. Although this age group is often less vulnerable, they also often comprise the primary breadwinners of families and thus each case of malaria means a loss of precious income through payment for treatment or lost labor time. In addition, drug-resistant strains of the disease have been on the rise in the border regions of the country. This can be caused by exposure to poor quality medicine, or more commonly failure to comply with medication directions. Mobile and migrant workers are particularly at risk because they work in the wooded border regions of Cambodia with high incidence, they often come from areas with less incidence of malaria, and they often work through the night.
PfD is working with the Global Fund in Kratie province to create an Early Warning System which will create a database tracking the emergence of drug-resistant cases. In order to do this, a network of PfD staff, volunteers, and partners have to draw and test blood samples from patients, and submit them for verification. It is this network that is the heart of PfD’s Regional Artemisinin Project.

Ry Monika
Kratie is among the poorest provinces in Cambodia, so those who contract malaria are sometimes unable to afford a visit to a private clinic. However, if they do choose the private clinic route, they will have the pleasure of seeing Miss Ry Monika. At her clinic, she will administer medicine and take a blood sample for a PfD staff member to collect. At this private clinic, the policy does not include a follow up with the patients. Reaching patients after they leave can be a key challenge, as many do not have phones or adequate service.

Ra Sarvuth on left
If a patient makes their way to the public clinic, Mr. Ra Sarvuth will take a blood sample and request the patient returns in 2 weeks. During this time, the blood sample has been collected by PfD staff and analyzed. Mr. Sarvuth works diligently to contact those who do not return.

Bin Soth
With the help of trained Volunteer Malaria Workers (VMWs), all who need assistance can be treated and tested. Bin Soth has been a VMW since 2004 and has worked diligently with PfD on other malaria control programs like net distribution and education campaigns. He has been trained by PfD on health education and behavior change communication (BCC) and has also been trained and provided medicines by the national program. Bin Soth also collects blood samples which are collected by PfD staff. If the malaria is a serious case or doesn’t improve then he refers the patient on to further care at a hospital or health center. Within the village that Bin Soth works and lives, he covers about 75 families over an area of 2-3km.

Tin Tak
Tin Tak has been a VMW since 2004 in the village of Batheuy, where her coverage area is about 3km. Like Bin Soth, Tin Tak takes blood samples for PfD to collect and she refers more complex cases and pregnant women on to hospitals and health clinics. However, the nearest health center is 23km away and the road in very poor condition. Therefore, the work she does in her community is vital to those who cannot make that trip.

Sreang Thavy center; Wife to left; One of their 5 children in front; PfD staff
Our VMWs are passionate about serving their friends, family and communities. They are proud to make every PfD meeting to keep current on our malaria prevention and control programs. Their service has been invaluable to beneficiaries like Sreang Thavy. Sreang Thavy has repeatedly contracted malaria due to his work in the nearby forest. When we met Sreang, he was sick for the 3rd time in just one year. After returning home from the forest, he was feeling very sick with a fever. At that point he knew he had to go to the local health post where they took a blood sample. It takes a while to recover enough strength to return to working in the forest, and this time can be economically damaging as he is unable to work and his family of 7 has no other source of income.

Kheng Phyreth and Im Ratana
Working tirelessly to prevent malaria in their community is PfD’s local staff based in Kratie province, such as Kheng Phyreth and Im Ratana. They map beneficiaries, collect samples from the clinics and VMWs, and maintain relationships with our partners. They often work long hours, having to reach remote areas on motorcycle. They are key members of the PfD team, working at the local level to achieve sustainable outcomes.
I first learned about PfD when PfD conducted malaria event and malaria education activity in my village using mobile video show. PfD also conducted many other community programs and training such as WASH, nutrition, child survival, agriculture, and chicken raising in my community. In 2013, PfD selected and trained me as Mobile Malaria Worker where I gained the knowledge and skills to provide malaria health education, diagnosis and treatment to my community members.
I am so proud to do this volunteer work.
 I have gained a lot of recognition and respect from the community members, my family, health center staff and the local authorities. I was so impressed with the malaria education activity; it informed and educated me and the community members on how to protect ourselves from malaria and where we can seek treatment when we are infected. Because I live in a malaria endemic village with lack of clean water, I am particularly passionate about malaria and WASH program of PfD’s work.
I have gained a lot of recognition and respect from the community members, my family, health center staff and the local authorities. I was so impressed with the malaria education activity; it informed and educated me and the community members on how to protect ourselves from malaria and where we can seek treatment when we are infected. Because I live in a malaria endemic village with lack of clean water, I am particularly passionate about malaria and WASH program of PfD’s work.
Our work saved our lives.
I think others should join the PfD family because PfD is the oldest NGO in Kratie Province in Cambodia and is implementing community development work to improve the quality and save lives of community members, particularly the vulnerable ones.
Throughout all of December we will be sharing stories from our staff, board, partners, and others from around the globe. We can’t wait to share all of the hopeful, engaging, and positive stories from our work. We will be using the hashtag #IamPfD on Facebook, Twitter and LinkedIn.

Be sure to share the posts that you find engaging and inspiring with friends and family and don’t forget to donate and take an #unselfie of you making a donation and share it with us and use the #IamPfD for a chance to win prizes from PfD.
Ms. Nub Chin and her family currently live in the malaria endemic forest village of Chhour Krang in Thmey commune, Snoul district, Kratie Province. With her family she lives in a village impacted by deforestation and climate change. Many of her fellow villagers are smallholder farmers who work on their farms daily in order to make a living. Malaria significantly impacts their work-life when it goes untreated.
 Although malaria is easy to treat, it is a problem for many, like the Chin family, who do not have access to health center or health practitioners. Like many in her village, Ms. Nub Chin has personally experienced dealt with malaria. Ms. Nub Chin and her daughter frequently got malaria in part because they didn’t understand the causes of it nor did they know how to prevent it. They believed that a spirit caused malaria and sought treatment from a traditional healer (Kru Khmer) leaving their condition un-treated.
Although malaria is easy to treat, it is a problem for many, like the Chin family, who do not have access to health center or health practitioners. Like many in her village, Ms. Nub Chin has personally experienced dealt with malaria. Ms. Nub Chin and her daughter frequently got malaria in part because they didn’t understand the causes of it nor did they know how to prevent it. They believed that a spirit caused malaria and sought treatment from a traditional healer (Kru Khmer) leaving their condition un-treated.
When they got sick with malaria, Ms. Nub Chin and her family were left with two options: 1. Spend a lot of money on transportation to reach the public health center dozens of kilometers away or 2. Seek treatment from the private health provider which is closer, but more expensive.
Ms. Nub Chin was motivated to change this!
After attending the malaria health education training provided by PfD, Ms. Nub Chin learned about the cause of malaria infection and treatment options. After the training, she expressed interest in volunteering to help her village. With training and support from PfD, Ms. Nub Chin became a Village Malaria Worker. As a Village Malaria Worker, Ms. Nub Chin has not only helped protect her family from malaria infections, but she has helped all the villagers, particularly the vulnerable ones, from malaria infections. In addition, she is able to save the money that she would have spent previously on malaria treatment.
Ms. Nub Chin is not only a trained Village Malaria Worker who provides malaria education, diagnosis and treatment in her village, but she has also offered to take her motorcycle to other nearby villages to provide education, diagnosis and treatment to other key affected population such as forest workers, seasonal migrant workers and smallholder farmers.
In the simplest of terms, Ms. Nub Chin is saving lives.
 Her motivation and dedication have helped prevent and treat hundreds of malaria cases. Because of women like Ms. Nub Chin, families in her village and surrounding villages are able to continue farming and save the money that would have otherwise been spent on malaria treatment to help feed their families and educate their children. Per month, Ms. Nub Chin provides health education to about 20 villagers on average, conducts around five blood tests among malaria suspected cases to screen for malaria, and provides treatment to all confirmed malaria cases.
Her motivation and dedication have helped prevent and treat hundreds of malaria cases. Because of women like Ms. Nub Chin, families in her village and surrounding villages are able to continue farming and save the money that would have otherwise been spent on malaria treatment to help feed their families and educate their children. Per month, Ms. Nub Chin provides health education to about 20 villagers on average, conducts around five blood tests among malaria suspected cases to screen for malaria, and provides treatment to all confirmed malaria cases.
Only with the leadership and dedication of local volunteers will we be able to tackle some of the biggest health challenges facing our world today. PfD strongly believes that Ms. Nub Chin is an example of the dozens of other local volunteers in Cambodia and around the world.
Throughout all of December we will be sharing stories from our staff, board, partners, and others from around the globe. We can’t wait to share all of the hopeful, engaging, and positive stories from our work. We will be using the hashtag #IamPfD on Facebook, Twitter and LinkedIn.

Be sure to share the posts that you find engaging and inspiring with friends and family and don’t forget to donate and take an #unselfie of you making a donation and share it with us and use the #IamPfD for a chance to win prizes from PfD.
Greetings from Geneva,
My journey with Partners for Development (PfD) has allowed me to see the organization from the inside out; therefore, I wanted to reach out to you and share my story. I have been working in the relief and development field for over 25 years and had the privilege of working with PfD from 1994 to 2002. I served at their headquarters and in two countries (Somalia and Cambodia) and several years ago I was elected to the Board of Trustees. Though my role has changed, my dedication and resolve for PfD has not. I encourage you to get to know the organization better and I have no doubt that you will come to love and support the organization in the same ways that I have.
My friends and colleagues often ask why I am so gung-ho about PfD. PfD’s tendency to work “off the tarmac” in oftentimes remote and unforgotten parts of the world sets them apart. When I served as PfD’s Country Director in Cambodia, our community health and development activities focused on the distant, difficult to access provinces in the Northeast. Nearly all our staff and resources were dedicated to serving these provinces and PfD teams were primarily comprised of people from these provinces. Many of the communities in which PfD worked were accessible only by long, arduous motorbike trips. Fun fact: PfD was the first major distributor of mosquito nets in the region.
PfD’s flat hierarchy and the small but dedicated headquarters staff make them nimble and extremely responsive to the field teams and the communities in which they work. Did you know that PfD’s Silver Spring office operates with a team of 6? I like the fact that a technical support officer in Nigeria can send an email to PfD’s Executive Director and expect a timely response from him. There is little to no bureaucracy and that is how I know my donation has the greatest impact.
I am proud to be formally affiliated with PfD and urge you to learn more about how YOU can support us!
Thank you,
Michael Chommie
Geneva
Throughout all of December we will be sharing stories from our staff, board, partners, and others from around the globe. We can’t wait to share all of the hopeful, engaging, and positive stories from our work. We will be using the hashtag #IamPfD on Facebook, Twitter and LinkedIn.

Be sure to share the posts that you find engaging and inspiring with friends and family and don’t forget to donate and take an #unselfie of you making a donation and share it with us and use the #IamPfD for a chance to win prizes from PfD.

PfD has worked to eradicate malaria (What Do You Know about Malaria?) in Cambodia by targeting interventions and projects towards migrant and mobile populations (MMPs), who make up a large percentage of the populations infected with and transmitting drug-resistant malaria in the Greater Mekong Subregion (GMS region, which includes Cambodia, Laos, Myanmar, Thailand, Vietnam, and Yunnan Province of China). The migratory nature of these populations and subsequent lack of access to or desire for health services enable both the transmission of resistant malaria from already-infected environments to malaria-free environments and also the cultivation of environments that enable vector-breeding.

The Main Cause: Treatment Failure
The incidence of drug-resistant malaria has been identified in considerably higher percentages in certain border provinces of the GMS region, such as the Thailand-Cambodia border. Most of the recently emerging malaria along this border is from migrants, who most often develop drug-resistant malaria due to treatment failure. These migrants often travel unsheltered and become exposed to uninhibited transmission. But because they are often unregistered, their fear of deportation or arrest can deter them from seeking medical care from a public hospital (WHO Quarterly Newsletter 2010). Instead, infected individuals turn to less effective drugs from unofficial vendors, which don’t fully eradicate the parasites and rather leave them desensitized to more effective treatments (The development and spread of drug-resistant malaria, W.H. Wernsdorfer) .
For other migrants, existing health facilities are rather inaccessible from their remote locations; in western Cambodia, specifically, a large proportion of malaria transmission is associated with migrant populations that visit forested areas, where they are missed by teams that conduct screening and treatment regimens. Even if some migrants do seek treatment, it is difficult for health workers to regulate them, since their mobile lifestyles often lead them to move onwards once they stop experiencing symptoms, even if their treatment is not complete. As a result, asymptomatic people, such as partially-immune migrants or individuals undergoing treatment, don’t seek medical help or discontinue treatment early, but continue to transmit the resistant parasite in the environments they enter (WHO) .
Why are MMPs more susceptible to drug-resistant malaria?
Partially-immune or nonimmune populations moving from low-transmission areas to high-transmission areas are generally more susceptible to the disease than resident populations who are already accustomed to it. Subsequent migration from high-transmission regions back to low-transmission regions allows for the introduction or re-introduction of the drug-resistant disease to previously malaria-free environments (IOM Global Report) . MMPs that have been displaced by conflict or natural disasters are particularly vulnerable to this kind of transmission, since they often move across larger regions or countries.
Growing economic disparities motivate the poor to migrate in search of jobs, perpetuating the negative effects of large-scale population increase and rapid urbanization. The likelihood of transmission increases as more people congregate in places with poor housing and shelter, a lack of proper sanitation or sewage systems, and unprotected water reservoirs that enable vector-breeding and increase the risk of human-vector contact (NIH). So while investments in road infrastructure and travel technology provide accessible routes for movement, they also expose communities to new environmental factors that can increase the transmission of drug-resistant malaria and the proliferation of vectors carrying the drug-resistant parasites (IOM Global Report).
PfD’s Response
To address this problem of drug-resistant malaria in Cambodia, specifically, PfD conducted a survey among MMPs in Cambodia’s Kratie and Koh Kong provinces in order to better assess their needs related to the disease (see PfD’s blog post). Based on the survey results, PfD is working to design more effective, targeted programs that can help reduce the high incidence of resistant malaria among these vulnerable mobile and migrant populations.

What are the signs or symptoms of malaria? How do people get malaria? How do people prevent malaria? These questions were recently asked as part of a Knowledge, Attitude, and Practice survey conducted by PFD in the Kratie and Koh Kong provinces of Cambodia. 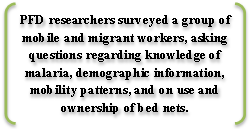
Our goal: to determine what the malaria affected populations knew about the mosquito-borne infectious disease. PFD is now using the data to get a better picture of the needs of the mobile and migrant populations (MMP) and, as a result, implementing better targeted programs.
So what did we find?
 97% of the workers have heard of malaria.
97% of the workers have heard of malaria.- When asked about the signs and symptoms that make them suspect malaria, 84% mentioned chills, 21.7% headache, almost 20% fever and about 16% sweating.
- 8.4% of respondents didn’t know signs or symptoms related to malaria.
- 92% of workers have at least one type of mosquito net (bed net or hammock net), but only half of those nets are insecticide treated nets (ITN).
- An estimated 69% of the workers slept under a treated net the previous night: 23% slept under an ITN bed net or hammock net and 46% under a long lasting insecticide-treated net (LLIN).
- Only 39% of workers own either an ITN or an LLIN and slept under it the previous night.
Next steps
Currently, PFD is working to eliminate malaria in Cambodia with funding from the Global Fund to Fight AIDS, Tuberculosis and Malaria. An integral part of PFD’s program is distributing insecticide-treated bed nets (ITNs). According to the CDC, ITNs have been shown to be very effective in the fight against malaria. Since the use of nets reduce the number of mosquitos and the mosquitos’ lifespan, if used by over 50 percent of a community, the nets will have a positive effect, helping to even protect those community members without nets. Since 2006, PFD has distributed nets which cover over 120,000 people in the Kratie and Koh Kong provinces in Cambodia.

To address the areas of weakness identified through the survey, our current programs will be modified to help increase ownership of bed nets and providing on-site programs to treat nets with insecticide. PFD is committed to continually monitoring and evaluating the local needs of the community along with the effectiveness of our interventions, and through this survey, can be at the forefront of developing new intervention strategies tailored to specific populations.
In recent years, PFD has focused on the mobile and migrant populations (MMP) who are at higher risk for malaria from their work in forest areas. Based on the 2008 census, it was estimated that 40,000 to 70,000 people migrated to malaria villages or areas, with about 25% of them non-immune to malaria (Ref MMP report 2010). Targeting MMPs is critical to stopping the spread of malaria, as the recent emergence and spread of antimalarial resistant parasites has been linked to population movement between non-malaria areas to malaria endemic areas.
PFD Recommendations for Cambodia Malaria Program

Apart from the provision of bed nets, PFD also works to educate the population: From 2012 to 2014 PFD reached over 300,000 people through community based malaria health education, 57,132 school children through school-based malaria prevention interventions, and provided training for over 2000 village health volunteers. Additionally, the survey reported that in 2013 80% of individuals correctly answered malaria related questions during community quiz events and 95% of the children who participated in the school based programs passed along the information on malaria prevention to their family, friends, or other community members through various activities.
Read more about PFD, our work to fight Malaria in Cambodia, and our other health projects.

Multi-drug resistant (MDR) malaria along the Cambodia-Thailand border continues to be a public health challenge. With the recent Ebola outbreak bringing to light the dangers of Partners for Development (PFD) with support from The Global Fund to Fight AIDS, Tuberculosis and Malaria (The Global Fund) is working to eliminate malaria in Cambodia, with special focus on containing drug resistant malaria. Cambodia has seen a significant decrease in malaria cases and deaths over the past decade which has been linked with the efforts of The Global Fund, in part due to PFD’s work in the villages most exposed to Malaria.our increasingly mobile global population combined with infectious diseases, many are fearful of what will happen if the new resistant strain of malaria reaches the rest of South East Asia and Africa. If MDR malaria reaches Africa, experts warn it will cause a severe health crisis. With an estimated 2.13 million people at risk for malaria in Cambodia, and the emergence of multi-drug resistance malaria, continuing the fight against malaria in Cambodia is a primary public health concern.
PFD uses a community based strategy: building the capacity of community level partners empowering those partners to sustainably undertake malaria prevention programs in the communities. Currently, PFD builds local capacity by training local Mobile Malaria Workers (MMW) to assess the needs of their communities and manage the distribution of malaria prevention backpacks. These subsidized backpacks, as shown in the photos, which are distributed through a voucher system include: insect repellent, flash light, a long lasting insecticide hammock (LLIH) or net (LLIN), and prevention and care information.

PFD is working with the highest risk population, the mobile and migrant populations (MMP) and those who work in the forests in Kratie province, helping to track and prevent malaria. Targeting the MMP population is critical to stopping the spread of malaria, as population movements from non-malaria endemic areas to malaria endemic areas in Cambodia are one of the main factors in the recent emergence and spread of antimalarial resistant parasites.
This program is one of many in PFD’s fight against malaria in Cambodia. PFD has spread awareness by training of health workers, teachers, volunteers and Community Councils in malaria prevention and reached thousands through radio broadcasts with malaria and health related messages. In 2014 alone, PFD trained 117 new primary school teachers, 10,150 children as peer educators in malaria health edu¬cation, and 43 new and existing Village Health Volunteers. Historically, PFD has trained over 1,300 teachers, benefitting 30,000 primary school students in health educa¬tion. PFD has also built local capacity of communities by providing funds to eleven Community Councils in Kratie and Koh Kong provinces so that local communities can design and implement malaria prevention activities tailored to the specific needs of their communities.
The global fight against Malaria has achieved some success over the past few years with incidence rates and mortality rates decreasing, resulting in an estimated 625 million fewer cases and 4.3 million fewer malaria deaths from 2001 to 2013 (WHO, 2014). Even with the substantial gains made against malaria, World Health Organization estimates remain high at 198 million malaria cases and 584,000 malaria deaths globally in 2013.
Follow the links to find out more about PFD’s work fighting malaria and programing in Cambodia.
Footnotes:
1. According to the Center for Disease Control and Prevention: Antibiotics and similar drugs, together called antimicrobial agents, have been used for the last 70 years to treat patients who have infectious diseases. Since the 1940s, these drugs have greatly reduced illness and death from infectious diseases. Antibiotic use has been beneficial and, when prescribed and taken correctly, their value in patient care is enormous. However, these drugs have been used so widely and for so long that the infectious organisms the antibiotics are designed to kill have adapted to them, making the drugs less effective. Many fungi, viruses, and parasites have done the same. Some microorganisms may develop resistance to a single antimicrobial agent (or related class of agent), while others develop resistance to several antimicrobial agents or classes. These organisms are often referred to as multidrug-resistant or MDR strains. In some cases, the microorganisms have become so resistant that no available antibiotics are effective against them.

